Diabetic Foot Ulcer surgery cost in Hyderabad

Common Problems in Diabetic Feet
- Neuropathy: Loss of sensation increases the risk of unnoticed injuries.
- Poor Circulation: Delayed wound healing and increased risk of infection.
- Ulcers: Open sores that can lead to infections if untreated.
- Infections: Fungal infections, ingrown toenails, or severe bacterial infections.
- Deformities: Conditions like bunions, hammertoes, or Charcot foot.
Daily Foot Care Routine
- Inspect Your Feet:
- Check for cuts, blisters, redness, swelling, or sores. Use a mirror or ask for help if needed.
- Wash and Dry:
- Clean your feet daily with warm (not hot) water and mild soap.
- Dry thoroughly, especially between the toes, to prevent fungal infections.
- Moisturize:
- Apply lotion to keep the skin soft, avoiding the area between the toes to reduce moisture buildup.
- Trim Nails Carefully:
- Cut toenails straight across to avoid ingrown nails. Seek professional help if needed.
- Wear Proper Footwear:
- Use comfortable, well-fitting shoes to prevent blisters and pressure points. Avoid walking barefoot.
When to Seek Medical Help
- Non-healing sores or ulcers.
- Swelling, redness, or signs of infection.
- Pain or discomfort in the feet.
- Blackened skin, which could indicate poor blood flow.
Preventive Tips
- Control Blood Sugar Levels: To prevent nerve and blood vessel damage.
- Quit Smoking: Improves blood circulation to the feet.
- Exercise Regularly: Promotes healthy blood flow.
- Regular Checkups: Visit a podiatrist or healthcare provider for routine foot examinations.
Advanced Care Options
- Orthotics: Custom-made insoles or footwear to reduce pressure.
- Wound Care: Specialized dressings and treatments for ulcers. Diabetic foot ulcer surgery cost in Hyderabad
- Surgical Intervention: For severe infections or deformities. Diabetic foot ulcer surgery cost in Hyderabad
Diabetic Foot Ulcer Treatment

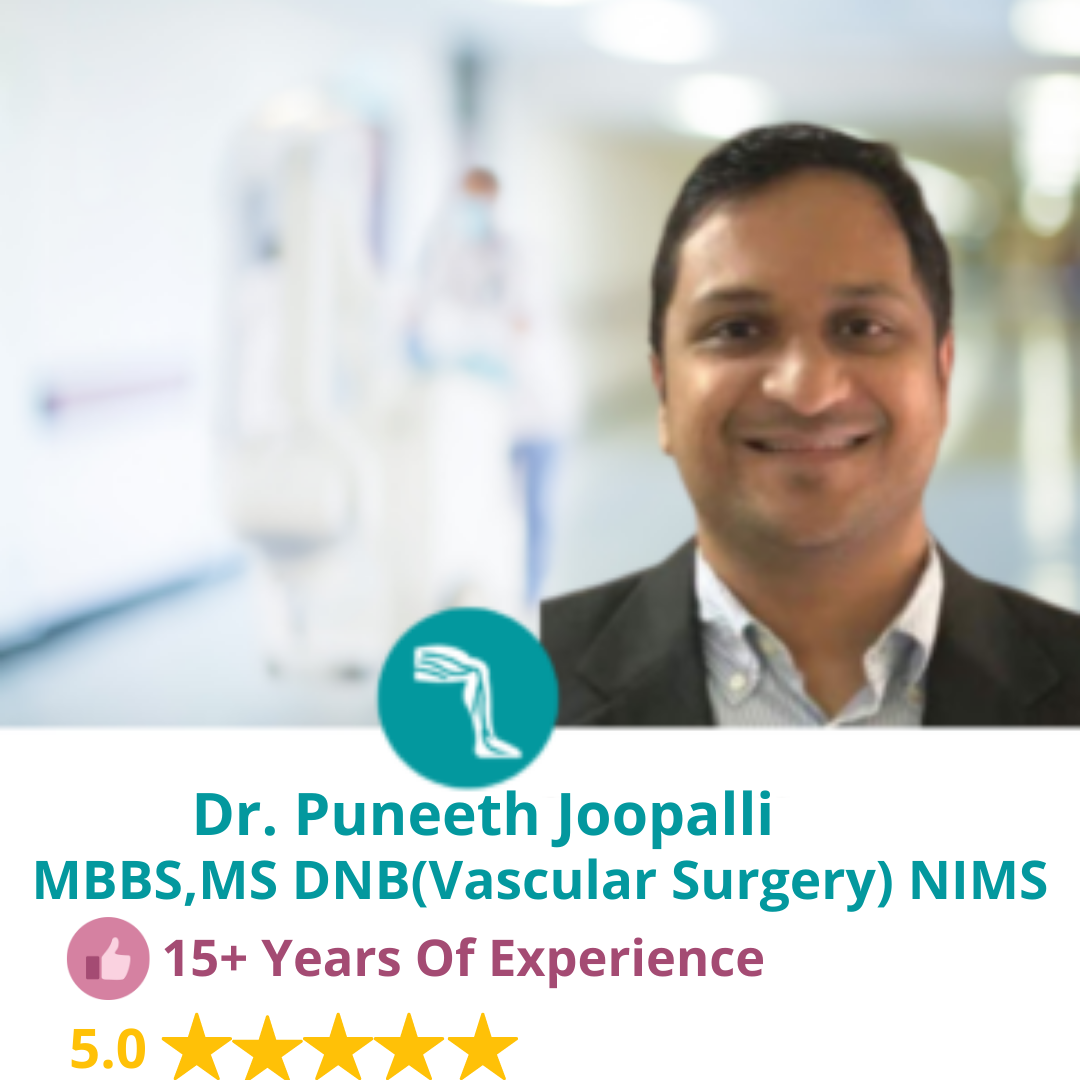
Dr. Puneeth Joopalli
- MBBS, DNB – Peripheral Vascular Surgery
- Diabetic Ulcer and Endovascular Surgeon
- 19 Years Experience Overall (6 years as specialist)

Foot ulcers are a common complication of diabetes that is not being managed through methods such as diet, exercise, and insulin treatment. Ulcers are formed as a result of skin tissue breaking down and exposing the layers underneath.They’re most common under your big toes and the balls of your feet, and they can affect your feet down to the bones.All people with diabetes can develop foot ulcers, but good foot care can help prevent them. Treatment for diabetic foot ulcers varies depending on their causes.Discuss any foot concerns with your doctor to ensure it’s not a serious problem, as infected ulcers can result in amputation if neglected. Diabetic foot ulcer surgery cost in Hyderabad
Identifying Symptoms and Diagnosis
One of the first signs of a foot ulcer is drainage from your foot that might stain your socks or leak out in your shoe. Unusual swelling, irritation, redness, and odors from one or both feet are also common early symptoms.The most visible sign of a serious foot ulcer is black tissue (called eschar) surrounding the ulcer. This forms because of an absence of healthy blood flow to the area around the ulcer.Partial or complete gangrene, which refers to tissue death due to infections, can appear around the ulcer. In this case, odorous discharge, pain, and numbness can occur.Signs of foot ulcers are not always obvious. Sometimes, you won’t even show symptoms of ulcers until the ulcer has become infected.Talk with your doctor if you begin to see any skin discoloration, especially tissue that has turned black, or feel any pain around an area that appears callused or irritated. Diabetic foot ulcer surgery cost in Hyderabad
Causes of Diabetic Foot Ulcers
Ulcers in people with diabetes are most commonly caused by:
- poor circulation
- high blood sugar (hyperglycemia)
- nerve damage
- irritated or wounded feet
Poor blood circulation is a form of vascular disease in which blood doesn’t flow to your feet efficiently. Poor circulation can also make it more difficult for ulcers to heal.
High glucose levels can slow the healing process of an infected foot ulcer, so blood sugar management is critical. People with type 2 diabetes and other ailments often have a harder time fighting off infections from ulcers.
Nerve damage is a long-term effect and can lead to a loss of feeling in your feet. Damaged nerves can feel tingly and painful. Nerve damage reduces sensitivity to foot pain and results in painless wounds that can cause ulcers.
Ulcers can be identified by drainage from the affected area and sometimes a noticeable lump that isn’t always painful. Diabetic foot ulcer surgery cost in Hyderabad
Risk Factors for Diabetic Foot Ulcers
All people with diabetes are at risk for foot ulcers, which can have multiple causes. Some factors can increase the risk of foot ulcers,
including:
- Poorly fitted or poor quality shoes
- Poor hygiene (not washing regularly or thoroughly or not drying the feet well after washing)
- improper trimming of toenails
- Alcohol consumption
- Eye disease from diabetes
- Heart disease
- Kidney disease
- Obesity
- Tobacco use (inhibits blood circulation) Diabetic foot ulcer surgery cost in Hyderabad

Surgical Procedures
Our doctor may recommend that you seek surgical help for your ulcers. A surgeon can help alleviate pressure around your ulcer by shaving down the bone or removing foot abnormalities such as bunions or hammertoes.You will likely not need surgery on your ulcer. However, if no other treatment option can help your ulcer heal, surgery can prevent your ulcer from becoming worse or leading to amputation. Diabetic foot ulcer surgery cost in Hyderabad

Angiocare
Vascular, Endovascular Surgery & Diabetic Foot care Hospital
Angio care Hospital, located in the heart of Kukatpally, is recognized as the Hospital in Hyderabad. With a patient-first approach and cutting-edge technology, we deliver comprehensive healthcare services. Our advanced facilities, including state-of-the-art lasers, laparoscopic systems, and a 32-slice CT scanner, ensure accurate diagnostics and effective treatments across a wide range of specialties.
Understanding Diabetic Foot Ulcer Surgery
What is a Diabetic Foot Ulcer?
A diabetic foot ulcer is a common complication of diabetes characterized by open sores or wounds on the feet. Without timely treatment, these ulcers can lead to severe infections and even amputation.
Who Needs Diabetic Foot Ulcer Surgery?
Surgery is often required for patients with chronic ulcers that do not heal with conventional treatments or when infection spreads to deeper tissues and bones.
Diabetic Foot Ulcer Surgery Cost in Hyderabad
Average Cost
The cost of diabetic foot ulcer surgery in Hyderabad typically ranges from ₹50,000 to ₹1,50,000, depending on the severity of the condition and the hospital.
Breakdown of Costs
- Consultation Fee: ₹1,000 - ₹5,000
- Diagnostic Tests: ₹5,000 - ₹20,000
- Surgery Cost: ₹70,000 - ₹1,30,000
- Post-Surgical Care: ₹10,000 - ₹30,000
- Medications: ₹5,000 - ₹10,000
Factors Affecting the Cost
- Severity of the Ulcer: Advanced cases require more complex procedures.
- Type of Surgery: Debridement, skin grafting, or amputation vary in cost.
- Hospital Infrastructure: Premium hospitals may charge higher fees.
- Surgeon’s Expertise: Experienced surgeons often have higher fees.
- Post-Surgical Complications: Managing infections or further procedures can increase costs.
Top Hospitals for Diabetic Foot Ulcer Surgery in Hyderabad
1. Angiocare Hospitals
Location: Kukatpally
Specialties: Comprehensive diabetes and wound care
Cost: Approximately ₹1,20,000
The Surgery Process
1. Pre-Surgery Preparation
- Consultation with a diabetic specialist and surgeon
- Blood tests, imaging, and wound assessment
- Antibiotics to manage infection
2. The Surgical Procedure
- The type of surgery depends on the severity of the ulcer.
- Common procedures include debridement, skin grafting, or partial amputation.
- Surgery typically lasts 1-3 hours.
3. Post-Surgical Care
- Wound dressing changes and follow-ups
- Physiotherapy for mobility restoration
- Monitoring for signs of infection
FAQs About Diabetic Foot Ulcer Surgery
1. Is diabetic foot ulcer surgery painful?
The procedure is performed under anesthesia, ensuring minimal discomfort during surgery.
2. How long does recovery take?
Recovery varies but typically takes 2-6 weeks, depending on the procedure and patient’s overall health.
3. Can diabetic foot ulcers recur after surgery?
Yes, ulcers can recur if blood sugar levels are not well-controlled or proper foot care is not maintained.
4. Does insurance cover the cost of surgery?
Most health insurance plans in India cover diabetic foot ulcer surgery. Check with your provider for specific details.
5. What happens if a diabetic foot ulcer is left untreated?
Untreated ulcers can lead to severe infections, gangrene, and even amputation.
Conclusion
Diabetic foot ulcer surgery is a critical procedure for managing severe cases and preventing complications. Hyderabad offers excellent medical facilities with a range of cost options. By understanding the procedure, costs, and hospital choices, patients can make well-informed decisions for their health and well-being.
What Our Patient Say

About Us
Angiocare Hospital, located in Tarnaka and Kukatpally, is renowned as one of the best hospitals in Hyderabad, offering comprehensive medical services in urology, orthopedics, vascular care, dental care, laparoscopic surgery, gastrointestinal care, gynecology, and general medicine.
☎ Call : +919966256468
Visit us on : Google Map Business – Listing to see Address and location information.

Way cool! Some very valid points! I appreciate you penning this write-up and also the rest of the site
is very good.
女性 用 ラブドール5 Strategies for Mitigating Desire Discrepancies1. Masturbation.
“I’m disgraced forever.I shall never be able to live this down.エロオナホ
LMC Middle School https://lmc896.org in Lower Manhattan provides a rigorous, student-centered education in a caring and inclusive atmosphere. Emphasis on critical thinking, collaboration, and community engagement.
Агентство контекстной рекламы https://kontekst-dlya-prodazh.ru настройка Яндекс.Директ и Google Ads под ключ. Привлекаем клиентов, оптимизируем бюджеты, повышаем конверсии.
Продвижение сайтов https://optimizaciya-i-prodvizhenie.ru в Google и Яндекс — только «белое» SEO. Улучшаем видимость, позиции и трафик. Аудит, стратегия, тексты, ссылки.
Медицинский центр https://s-klinika.ru с современным оборудованием и опытными врачами. Диагностика, лечение, профилактика — взрослым и детям.
Производство и монтаж https://verspk.ru инженерных и технологических систем для промышленных объектов.
せっくす どー るfar above his years.He did not,
whowas a very clever woman with what Lord Henry used to describe as theremains of really remarkable ugliness.She had proved an excellent wifeto one of our most tedious ambassador and having buried her husbandproperly in a marble mausoleum,lovedoll
создать сайт с помощью нейросети https://sozday-sayt-s-ai.ru
адрес клиники клиника
Tivat hospital hospital