What is an AV fistula?

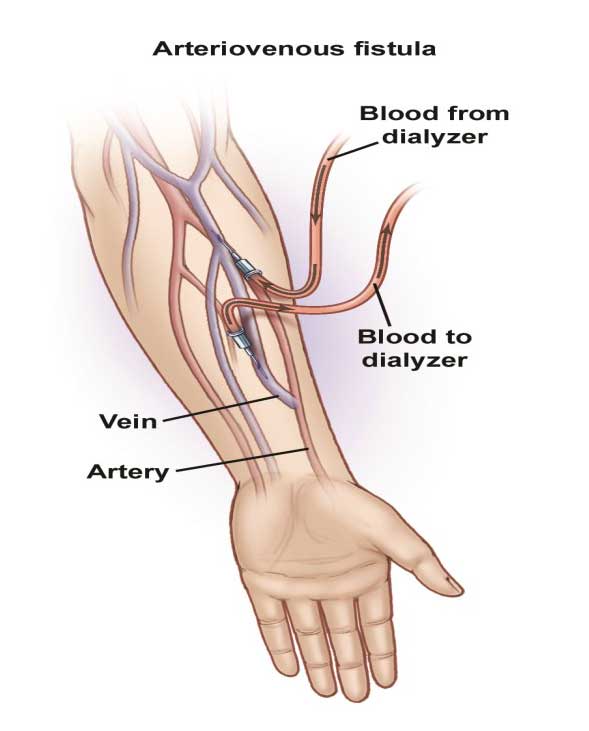
An AV fistula is a surgical connection made between an artery and a vein, c. An AV fistula is typically located in your arm, however, if necessary it can be placed in the leg. With an AV fistula, blood flows from the artery directly into the vein, increasing the blood pressure and amount of blood flow through the vein. The increased flow and pressure causes the veins to enlarge. The enlarged veins will be capable of delivering the amount of blood flow necessary to provide an adequate hemodialysis treatment. AV fistulas are the preferred vascular access for long-term dialysis because they last longer than any other dialysis access types, are less prone to infection and clotting, and can be relied upon for predictable performance.
An arteriovenous (AV) fistula is an abnormal connection between an artery and a vein. Normally, blood flows from your arteries to your capillaries, and then on to your veins. Nutrients and oxygen in your blood travel from your capillaries to tissues in your body.
With an arteriovenous fistula, blood flows directly from an artery into a vein, bypassing some capillaries. When this happens, tissues below the bypassed capillaries receive less blood.
Arteriovenous fistulas usually occur in the legs, but can develop anywhere in the body. Arteriovenous fistulas are often surgically created for use in dialysis in people with severe kidney disease.
A large untreated arteriovenous fistula can lead to serious complications. Your doctor monitors your arteriovenous fistula if you have one for dialysis.
The first step in AV fistula creation is to evaluate your blood vessels (veins and arteries), to ensure they are healthy enough to support a fistula. The first step in the evaluation will be a physical examination of your arms performed by our vascular specialist. The next step will involve the use of non-invasive or minimally invasive tests such as ultrasound, and possibly an angiogram to determine the size and depth of your arteries and veins. These tests will determine whether or not your blood vessels are able to support an AV fistula.
Symptoms
Small arteriovenous fistulas in your legs, arms, lungs, kidneys or brain often won’t have any signs or symptoms and usually don’t need treatment other than monitoring by your doctor. Large arteriovenous fistulas may cause signs and symptoms.
Arteriovenous fistula signs and symptoms may include:
- Purplish, bulging veins that you can see through your skin, similar to varicose veins
- Swelling in the arms or legs
- Decreased blood pressure
- Fatigue
- Heart failure
A significant arteriovenous fistula in your lungs (pulmonary arteriovenous fistula) is a serious condition and can cause:
- A bluish tinge to the skin
- Clubbing of fingers (the fingertips spread out and become rounder than normal)
- Coughing up blood
An arteriovenous fistula in your gastrointestinal tract can cause bleeding in your digestive tract.
If you have any of these signs and symptoms and think you might have an arteriovenous fistula, make an appointment to see our doctor. Early detection of an arteriovenous fistula may make your condition easier to treat. It also may reduce your risk of developing complications, including blood clots or heart failure.
Causes
- Injuries that pierce the skin. An arteriovenous fistula may occur if you have a piercing injury, such as a gunshot or stab wound, on a part of your body where a vein and artery are side by side.
- Being born with an arteriovenous fistula (congenital). The exact reason why isn’t clear, but in some babies, the arteries and veins don’t develop properly in the womb.
- Genetic conditions. Arteriovenous fistulas in the lungs (pulmonary arteriovenous fistulas) can be caused by a genetic disease (Osler-Weber-Rendu disease, also known as hereditary hemorrhagic telangiectasia) that causes blood vessels to develop abnormally throughout your body, but especially in the lungs.
- Dialysis-related surgery. People who have late-stage kidney failure may have an arteriovenous fistula surgically created in the forearm to make it easier to perform dialysis.
Risk factors
In addition to certain genetic or congenital conditions, the following risk factors may make you more likely to develop an arteriovenous fistula:
- Being female
- Cardiac catheterization, especially if the procedure involves blood vessels in your groin
- Certain medications, including some blood thinners (anticoagulants) and medications used to control bleeding (anti-fibrinolytics)
- High blood pressure
- High body mass index (BMI)
- Older age
Complications
Left untreated, an arteriovenous fistula can cause complications, some of which can be serious. These include:
- Heart failure. This is the most serious complication of large arteriovenous fistulas. Blood flows more quickly through an arteriovenous fistula than it does through normal blood vessels. As a result, your heart pumps harder to make up for the increase in blood flow. Over time, the increased workload on your heart can interfere with how the heart works, leading to heart failure.
- Blood clots. An arteriovenous fistula in your legs can cause blood clots to form, potentially leading to deep vein thrombosis, a painful and potentially life-threatening condition if the clot travels to your lungs (pulmonary embolism). Depending on where your fistula is, it can lead to a stroke.
- Leg pain. An arteriovenous fistula in your leg can cause pain in your leg (claudication), or can worsen pain you already have.
- Bleeding. Arteriovenous fistulas may lead to bleeding in your gastrointestinal system.
